Total Anomalous Pulmonary Venous Return:
Clinical:
TAPVR results from embryologic failure of the common pulmonary vein to join the posterior wall of the left atrium [4]. In TAPVR the pulmonary veins from both lungs drain into the systemic venous circulation (ie: to the right atrium). A right to left communication (ASD, patent foramen ovale, VSD, PDA, or combination of lesions) is necessary for survival. The most common type of communication is an ASD of the sinus venosus type. Neonates with supracardiac and cardiac TAPVR have mild to moderate cyanosis- depending on the amount of intracardiac mixing and the streaming of flow across the ASD [2]. As the pulmonary venous resistance decreases, the pulmonary blood flow increases even more, resulting in a larger left-to-right shunt [2]. Tachypnea becomes more prominent, followed by diaphoresis with feeding [2]. Infradiaphragmatic TAPVR presents differently- these neonates feed poorly and become hemodynamically unstable. Respiratory distress develops requiring intubation soon after birth [2]. Approximately one-thrid of patients with TAPVR have other associated cardiac lesions- many have heterotaxy syndrome- particularly asplenia [3].Without surgical correction, most affected patients will die in the first year of life. Surgical correction is usually postponed until the patient is at least one month of age as there is decreased mortality following repair between the ages of one month and one year. There are 4 types of anomalous pulmonary venous return:
Type I- Supracardiac: This is the most common variety accounting for 50-55% of cases. Supracardiac TAPVR can be divided into:
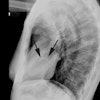
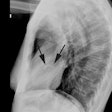
i) Drainage into derivatives of the left cardinal system (supracardiac vein). Typically- four anomalous pulmonary veins (two from each lung) converge directly behind the left atrium and form a common ascending vein known as the vertical vein [3]. The vertical vein passes posterior to the left atrial apendage and anterior to the left pulmonary artery and the left main bronchus to join the innominate vein [3,4] (a left vertical vein [or left SVC] to left inominant (brachiocephalic) vein connection exists due to persistence of the left anterior cardinal vein). Note: The left SVC normally drains into the coronary sinus, however, this connection is lost in patients with TAPVR. The inominate vein and SVC are dilated [4]. A "Snowman" configuration is produced on the CXR where the head represents the dilated SVC (on the right) and engorged left vertical vein (on the left) and the body is due to right atrial and right ventricular enlargement. On the lateral exam the left SVC is seen anterior to the trachea and produces a pretracheal density. There is always an ASD or patent foramen ovale to provide flow to the left side of the heart [4]. Venous obstruction in type I TAPVR is uncommon, but extrinsic obstruction may occur if the vertical vein courses between the left pulmonary artery anteriorly and the left main bronchus posteriorly [3].
ii) Less commonly, drainage is into derivatives of the right cardinal system such as the superior vena cava or azygous vein. This occurs due to failure of the common pulmonary vein to form or become completely incorporated into the left atrial wall, with persistence of drainage of the pulmonary system into the right cardinal system.
Type II- Cardiac: (30% of cases [3])- the pulmonary veins join to drain to either:
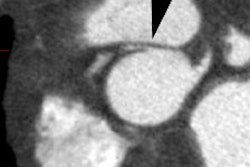
A. Coronary sinus (site of confluence of coronary veins): This is the most common site of connection [5]. Pulmonary veins connect to the coronary sinus which dilates.Echocardiography shows a characteristic "whale's tail" appearance [4].
B. Right Atrium: This is the next most common site of connection [5]. Pulmonary veins empty directly into the right atrium posteriorly. This form of TAPVR presents no specific signs on plain film.
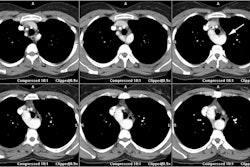
Type III- Infracardiac: (12-13%) There is an infracardiac or infradiaphragmatic connection via a persistent communication with the umbilical-vitelline venous system. The pulmonary veins join to form a large single vein behind the left atrium which descends through the esophageal hiatus (anterior to the esophagus [3]) to join the portal vein (this is the most common connection and typically occurs at the confluence of the splenic and superior mesenteric veins [4]), hepatic veins, ductus venosus, or IVC. This condition is almost always associated with obstruction of the pulmonary venous drainage due to the long course and high pressures. As a result of obstruction of pulmonary venous flow, patients are dyspnic and severely cyanotic at birth, and the cyanotic episodes are exacerbated by feeding (the bolus compresses the pulmonary vein near the distal esophagus). Death usually occurs within a few days. Infradiaphragmatic TAPVR is associated with Asplenia syndrome (80%). On CXR there is severe interstitial pulmonary edema with a usually normal sized (or enlarged) heart. There is thymic atrophy and pleural effusions may be seen. Severe obstruction will result in persistent fetal circulation with R->L shunting and therefore classic interstitial edema may not be seen.
Type IV- Mixed form of TAPVR- there are anomalous venous connections at two or more levels. This is the least common form or TAPVR (9-11% of patients) [5]. In the most common pattern there is a combination of supracardiac and cardiac connection with a vertical vein draining into the left innominate vein, and the anomalous vein or veins from the right lung drain into the right atrium or the coronary sinus [3,5]. This pattern is associated with other major cardiac lesions [3].
X-ray:
On CXR there will be shunt vascularity, cardiomegaly, a prominent PA segment, and a normal sized left atrium. Because of the increased return of blood to the right atrium, dilatation of the right atrium, right ventricle, and pulmonary arteries occurs [2]. The left heart structures are normal [2].REFERENCES:
(1) Seminars in Roentgenology 1989; Budorick NE, et al. The
pulmonary
veins. 24 (2) Apr: 127-140 (Review. No abstract available.)
(2) Pediactric Clinics of North America 1999; Grifka RG. Cyanotic congential heart disease with increased pulmonary blood flow. 46(2): 405-425
(3) Radiographics 2007; Ferguson EC, et al. Classic imaging signs
of
congenital cardiovascular abnormalities. 27: 1323-1334
(4) Radiographics 2012; Vyas HV, et al. MR imaging and CT
evaluation
of congenital pulmonary vein abnormalities in neonates and
infants. 32:
87-98
(5) Radiographics 2017; Hassani C, Saremi F. Comprehensive cross-sectional imaging of the pulmonary veins. 37: 1928-1954