Papillomatosis, Laryngeal
Clinical:
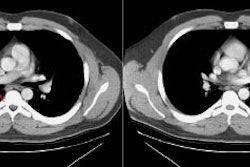
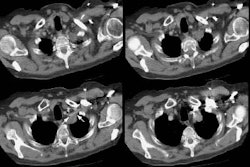
Laryngeal papillomatosis is secondary to a viral infection from maternal condylomata acuminata (human papilloma DNA virus infection subtypes 6 and 11) at the time of delivery. The papilloma is the most common laryngeal tumor of childhood, but is rare in adults. Patients present with before age 5 with hoarseness or voice change (as the vocal cords are usually the first affected site), stridor, cough, and dyspnea/respiratory distress [6]. The papillomas generally localize to the larynx (95%), but can also be found in the trachea or proximal bronchi (5%), or in the distal lung (less than 2-3%). Distal involvement is more commonly seen in children, but lung lesions usually do not appear until 10 years after laryngeal involvement [3]. Lung involvement in the absence of laryngeal involvement is rare. Factors that increase the risk of pulmonary involvement include diffuse viral contamination and tracheobronchial dissemination of fragments related to tracheotomy or surgical microexcision [3].Pulmonary spread is characterized by multiple well defined nodules which frequently cavitate. The cavities usually have thin walls (2-3 mm thick) and may contain air-fluid levels. Pulmonary involvement can be fatal.
The disease cannot be cured, but may go into remission, particularly if involvement is limited to the larynx (uncomplicated cases of laryngreal papillomatosis tend to regress at puberty, but no regression of pulmonary lesions has been reported [3]) [6]. Treatment is immunotherapy with maternal transfer factor, and for pulmonary involvement alpha interferon, antiviral drugs, and growth inhibiting agents such as retinoids. Tracheobronchial and pulmonary involvement are associated with a worse prognosis [6]. Early onset disease and HP11 subtype are associated with a more aggressive course [6]. The mortality associated with pulmonary disease is about 57% because of respiratory failure, infection, and malignant transformation [6].
Carcinomatous transformation to squamous cell carcinoma can occur very rarely (about 0.5-2% of patients [3]), particularly in patients with human papillomavirus 11 subtype (but the incidence in HP11 patients can eb as high as 16%) [6] and there is also an increased risk following XRT. [1] The risk for malignant transformation also increases with smoking, age greater than 40 years, and infections with human papillomavirus 16 or 18 [5].
Solitary squamous cell papilloma of the tracheobronchial tree is less common than the multiple form and usually occurs in adults [4]. The lesion can arise de novo or it can be associated with cigarette smoking [4]. The lesion can infiltrate and become malignant [4].
X-ray:
Airway film may show multiple small tracheal nodules. Distal airway lesions may obstruct and can result in atelectasis.Pulmonary spread is characterized by multiple well defined slow-growing nodules that frequently cavitate and appear as cysts. The cavities usually have thin walls (2-3 mm thick) and may contain air-fluid levels, particularly if there is superimposed infection.
REFERENCES:
(1) J Thorac Imag 1995; 10: 180-198 (p.182-184)
(2) Radiology 1997; 204: 388
(3) Radiographics 2002; Gimenez A, et al. Unusual primary lung tumors: a radiologic-pathologic overview. 22: 601-619
(4) AJR 2006; Ko JM, et al. Benign tumors of the tracheobronchial tree: CT-pathologic correlation. 186: 1304-113
(5) Radiographics 2009; Park CM, et al. Tumors in the
tracheobronchial tree: CT and FDG PET features. 29: 55-71
(6) Radiographics 2018; Lichtenberger JP, et al. Primary lung tumors in children: radiologic-pathologic correlation. 38: 2151-2172