Overlapping or collapsed bowel loops are a common problem in gastrointestinal imaging. But accurate radiological diagnosis is crucial when it comes to small bowel disease, which tends toward nonspecific symptoms. Increasingly, radiologists are relying on MR enteroclysis in order to devise a more ideal way to study the small bowel.
"The principal advantage of conventional enteroclysis is that the jejunum and ileum can be optimally distended. Conventional enteroclysis also provides functional information by defining distensibility or fixation of the small bowel loops.... On the other hand, conventional enteroclysis gives only indirect information on the state of the bowel wall and its surrounding structures," wrote Dr. Heiz Werner Umschaden and colleagues from General Hospital Klagenfurt in Klagenfurt and the Karl-Franzens University Hospital in Graz, both in Austria (Radiology, June 2000, Vol. 215:3, pp. 717-725).
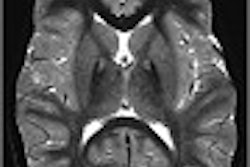
Umschaden’s group compared MR enteroclysis images with conventional enteroclysis, and surgical findings, in 30 patients with symptoms of either inflammatory bowel disease or small bowel obstruction (SBO). The small bowel enema consisted of 1,500-3,000 mL methylcellulose-water solution, administered with an electric infusion pump at a rate of 100-250 mL per minute.
All MR studies were performed on a 1-tesla Gyroscan ACS NT (Philips Medical Systems, Best, the Netherlands) with a single-shot, fast spin-echo, T2-weighted sequence applied to assess dynamic changes.
According to the results, MR enteroclysis was well tolerated by the patients (versus conventional enteroclysis, which brought on vomiting in some patients before the exam was completed) and provided adequate image quality and sufficient small bowel distension.
"There was exact agreement between MR enteroclysis and retrospective findings in all five patients who underwent surgery, and MR findings were identical to those at enteroclysis in all 18 patients, superior in six patients, and inferior in one patient," the authors wrote. "The inherent advantage of MR enteroclysis over conventional enteroclysis was related to the assessment of extraluminal disease," including Crohn’s disease, a jejunocolic fistula, and chronic phlegmon.
More recently, a group from Ludwig Maximilians University in Munich, Germany reported similar positive results with MR enteroclysis at the 2002 RSNA meeting in Chicago.
"Small bowel diagnosis is still a great challenge for all imaging modalities," said Dr. Karin Hermann. "Optimal distension of the small bowel is indispensable for diagnosis, especially in inflammatory bowel disease. Our goal was to find out how to optimize small bowel distension."
Hermann and colleagues used an online-monitored filling procedure under MRI fluoroscopic control and compared it to static MR enteroclysis after conventional fluoroscopic small bowel filling. The study population consisted of 20 patients who underwent static MR enteroclysis and conventional fluoroscopic filling, and 20 who had MR fluoroscopy with the online filling procedure. All imaging was done on a 1.5-tesla Magnetom Sonata scanner (Siemens Medical Solutions, Erlangen, Germany).
"The filling started outside the scanner for 10 minutes and then we continued inside the scanner," Hermann wrote.
MR fluoroscopy was performed with coronal, T2-weighted half-Fourier acquisition single-shot turbo spin-echo (HASTE) sequences. Postfilling, imaging was done with 3D contrast-enhanced gradient-echo sequences. Three independent readers rated the quality of small bowel distension.
The readers rated luminal distension as equal or better with online-monitored filling, according to the results. Moreover, all anatomic sections of the small bowel were sufficiently identified with MR fluoroscopy, Hermann stated. As a result, the number of failed readings because of collapsed small bowel loops was reduced.
"This leads us to conclude that dynamic MR fluoroscopy significantly improves the quality of distension and diagnostic reliability," Hermann said. "MR-fluoroscopic control for the filling procedure in small bowel enteroclysis appears to be superior to static MR enteroclysis."
Finally, another group from Germany, this time based at Christian Albrechts University in Kiel, also found dynamic MR enteroclysis as "feasible in the routine diagnostic work-up of the small bowel." They compared conventional enteroclysis, static MRI, and dynamic MR enteroclysis for the detection of small bowel stenoses.
For their study, 42 patients with Crohn’s disease or other suspected small bowel lesions were examined. Bowel filling was monitored on MR with four series of coronal, T2-weighted HASTE breath-hold sequences.
According to their results, static MRI performed within one hour after conventional enteroclysis showed insufficient bowel distension. In comparison, "dynamic MR enteroclysis led to controlled and complete bowel distension, which allowed for significantly better evaluation of normal bowel anatomy (and) revealed significantly more stenoses (42 out of 42 patients)." Additionally, dynamic MR enteroclysis helped physicians differentiate between fixed and non-fixed stenoses (RoFo. Fortschritte auf dem Gebiete der Rontgenstrahlen und der neuen bildgebenden Verfahren, September 2002, Vol. 174:9, pp.1158-1164).
These outcomes are promising, but "whether MR enteroclysis will readily replace currently used methods of small bowel imaging will depend on how this method can be integrated in the clinical setting," wrote Drs. Dean Maglinte, Evan Siegelman, and Frederick Kelvin in a Radiology editorial. Maglinte and Kelvin are from the Methodist Hospital of Indiana in Indianapolis; Siegelman is from the University of Pennsylvania Medical Center in Philadelphia.
They pointed out several advantages of MR enteroclysis that give it the potential to change how the small bowel is studied: functional information, soft-tissue contrast, direct multiplanar imaging, lack of ionizing radiation, and the ability to assess the severity of small bowel obstruction, which is frequently of great interest to referring physicians (Radiology, June 2000, Vol. 215:3, pp. 639-641).
One major disadvantage of MR enteroclysis, however, is the need for nasogastric intubation, which can cause severe patient discomfort. A way around this problem is for radiologists to consult with referring physicians early on so that the patient does not require repeat intubation, they said.
But "to be the primary method for investigation of small bowel disease, MR enteroclysis will have to provide reliable evidence of normalcy, allow diagnosis of early or subtle structural abnormalities, influence treatment decisions in patient care, and be cost-effective," they concluded.
By Shalmali PalAuntMinnie.com staff writer
February 5, 2003
Related Reading
German group optimizes barium-sulfate tagging in MR colonography, January 22, 2003
Italian study demonstrates value of MR in Crohn’s disease assessment, December 3, 2002
Video capsule endoscopy deemed superior to small bowel radiography, November 6, 2002
Copyright © 2003 AuntMinnie.com