Researchers in the U.K. have mined a large national stroke registry and identified risk factors for patients that may be involved in poor outcomes after endovascular thrombectomy (EVT).
A group led by Dr. Permesh Singh Dhillon of the University of Nottingham found that despite the complete success of endovascular thrombectomy (EVT) for acute stroke, 44% of patients experienced poor outcomes. Identifying factors contributing to these poor outcomes could ultimately improve patient care, according to the authors.
"Knowledge of these factors is important in determining modifiable risk factors for potential target therapies and for optimizing patient selection and care," the group wrote in an article published March 15 in the Journal of Stroke and Cardiovascular Diseases.
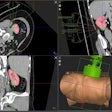
Thrombectomy is the gold standard treatment for large vessel occlusion (LVO) in acute ischemic stroke. It is a type of minimally invasive endovascular therapy in which interventional radiologists remove blood clots from the brain. This restores blood flow and reduces damage to brain tissue.
For reasons that yet remain unclear, patients may experience early neurological deterioration and intracranial hemorrhages as early as three months after the procedure. In this study, the researchers aimed to identify risk factors that could help predict these poor outcomes.
The group identified 2,132 of 4,383 patients (48.8%) with complete recanalization (restoration of blood flow) post-EVT, of which 948 patients (44.4%) developed poor outcomes. Data was collected from the Sentinel Stroke National Audit Program (SSNAP) registry, a national stroke registry that includes all hospitals admitting patients with acute stroke in England and Wales.
Based on a multivariable regression analysis, poor outcomes were associated with multiple baseline patient, imaging, and procedural factors, as follows:
- Age
- Admission NIHSS scores (a 15-item neurological examination stroke scale)
- Pre-stroke disability
- Onset-to-puncture and procedural times
- Presence of diabetes
- Use of general anesthesia
While some of these factors, such as increasing age and disability, can't be modified, "continued efforts to improve the time-to-treatment/recanalization and development of adjuvant therapies (e.g., neuroprotectants) while enhancing patient selection for EVT treatment should be considered," the group wrote.
The authors noted that the number of EVT cases performed per year steadily increased from 602 in 2017 to 1,607 in 2019-2020. While this equates to a small percentage of all acute stroke admissions per year, the trend highlights the importance of improving outcomes in these patients, the group wrote.
"Further prognostication studies are warranted to aid in the risk stratification and optimization of patient selection in an increasingly frail aging population," Dhillon and colleagues concluded.