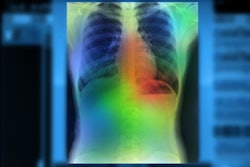
VIENNA - A deep-learning algorithm used with chest CT can help clinicians quantify patients' subcutaneous fat tissue levels on lung cancer screening -- and thus better predict disease outcomes, according to a presentation delivered on 29 February at ECR 2024.
The findings could help clinicians tailor patient care, said presenter Dr. Fabian Pallasch of University Medical Center Freiburg in Germany.
"[We found that] subcutaneous adipose tissue density at baseline and a decrease in subcutaneous adipose tissue volume and density within one year [were] associated with mortality beyond clinical risk factors, which may help to improve personalized risk assessment," he told session attendees.
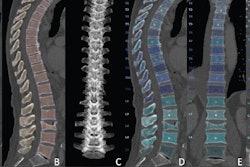
There's "increasing evidence that body composition is important for personalized prognostication in cardiovascular disease and lung cancer," Pallasch said, but most studies have focused on muscle, and little is known about the role adipose tissue can play. To address this knowledge gap, the investigators developed and tested a deep-learning model for quantifying 3D subcutaneous adipose tissue (SAT) on low-dose CT (LDCT) and investigated any associations between SAT measures and mortality among 26,144 participants in the National Lung Screening Trial (NSLT). Medical students under resident supervision used data from manual segmentations to develop the model, which consisted of 50 testing and 150 training samples.
Pallasch and colleagues analyzed CT exam results from study participants at baseline and at 12-month follow-up and quantified SAT volume (SATvol) and density (SATHU). The study's primary outcome was all-cause mortality, with additional outcomes being lung cancer and cardiovascular mortality.
The team found the following:
- Of the total study cohort, 7% (1,839) died over a median follow-up of 6.5 years.
- At baseline imaging, only SAT density correlated with all-cause mortality after adjusting for risk factors such as age, sex, race, smoking status, pack years, hypertension, diabetes, past stroke, and myocardial infarction, with a hazard ratio of 1.07 (with 1 as reference).
- At 12-month follow-up, patients with a decline in SATvol or SAT density equal to or more than 10% had worse outcomes compared with those with stable SATvol or SAT density, with a hazard ratio of 1.94 for SATvol and 3.1 for SAT density (adjusted for the same risk factors).
- The model had a Dice Similarity Coefficient (DICE) score of 0.88.
| Body composition measures at baseline imaging generated by deep learning plus CT among lung cancer screening patients | |
|---|---|
| Measure | Baseline |
| BMI, kg/m2, mean | 28 |
| AT volume, mL, mean | 4788.5 |
| AT density, HU, mean | -90.5 |
| All-cause death | 7% |
| ASCVD | 1.8% |
| Lung cancer death | 1.6% |
Deep learning shows promise for opportunistic SAT assessment at lung cancer screening, Pallasch concluded.
Implementing a tool like the proposed deep-learning model into the electronic medical records could help for opportunistic screening of altered SAT," he told session attendees. "Extracting this information may be helpful to identify high-risk individuals and to reduce morbidity and mortality."
For more coverage from ECR 2024, please visit our RADCast.